ClarisHealth Highest-Designated Major Contender in Everest Group Payment Integrity Solutions PEAK Matrix® Assessment 2024
Leading provider of enterprise payment integrity technology for health plans included in industry analysis report. Position credited to its unique adaptability to address payer pain points at multiple stages of their payment integrity journey.
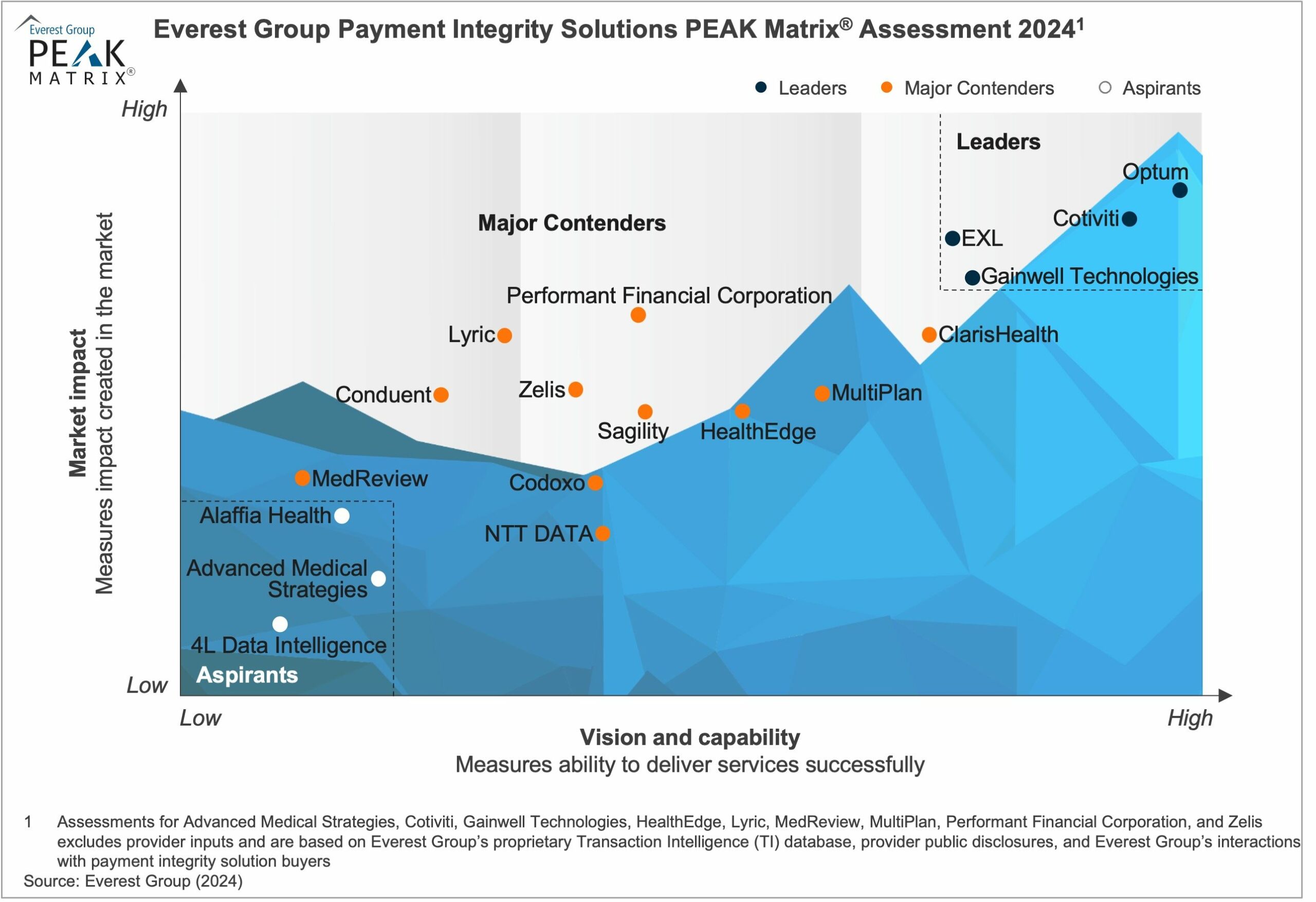
BRENTWOOD, Tenn., February 6, 2024 – ClarisHealth, provider of the industry’s leading enterprise payment integrity technology for health plans, announced today that it the highest-designated Major Contender in Everest Group’s Payment Integrity Solutions PEAK Matrix® Assessment 2024.
The PEAK Matrix measures market impact, vision and capability using proprietary information, provider public disclosures, and interactions with payment integrity solution buyers.
Ankur Verma, vice president at Everest Group, who contributed to the research said, “The increasing complexities in the payment integrity landscape is necessitating the demand for automated solutions capable of real-time error detection and comprehensive pre- and post-pay management.”
With its integrated technology platform Pareo®, ClarisHealth was noted in the research as a solutions provider having a dominant presence across most of the payment integrity value chain processes.
“ClarisHealth’s automation-enabled cloud-based platform solution has enhanced its ability to provide real-time data-driven insights, enabling healthcare payers to streamline prepay and post-pay tasks effectively,” Verma added. “Its unique adaptability to address payer pain points at multiple stages of their payment integrity journey has positioned it as a Major Contender in Everest Group’s Payment Integrity Solutions PEAK Matrix Assessment 2024.”
Tate McDaniel, the chief revenue officer for ClarisHealth, added that their enterprise technology supports a strategic shift in the payment integrity industry.
“Payers are seeing the benefits of modernizing their payment integrity operations with enterprise technology, and value the transparency and cost-savings that an integrated technology platform offers,” said McDaniel.
“There is a dynamic shift occurring in this industry, and we are proud to be at the forefront of reimagining claims cost containment activities. Our mission has always been to create a better way to drive claims payment accuracy.”
The study is designed to enable payers to identify suitable providers to transform their business processes and differentiate themselves. This is the second time that ClarisHealth has been named by Everest Group as a key player in the payment integrity solutions market.
To learn more about how ClarisHealth is creating a new paradigm for payment integrity, click here.
View source version at https://www.prweb.com/releases/clarishealth-highest-designated-major-contender-in-everest-group-payment-integrity-solutions-peak-matrix-assessment-2024-302053032.html
Now’s the time for total payment integrity
See the ClarisHealth 360-degree solution for total payment integrity in action.

